Learning Objectives
- Learn the Common Intestinal Parasites of dogs.
- Identify common treatments and methods of control to prevent these parasites.
Please consult a veterinarian before using any medications for the treatment or prevention of parasites.
Unit 1: Intestinal Worms
Roundworm (Toxocara canis)
The roundworm Toxocara canis has an unsegmented body with one digestive tract. The adult worms are yellow or white with pointed tips. This endoparasite feeds on the intestines of dogs; while the species Toxocara cati infects cats, and Toxascaris leonina infects both dogs and cats.
Toxocara canis is a zoonotic agent that can migrate to human tissues (visceral larva migrans). Toxocariasis is a disease that causes blindness in people.
Bitches can reinfect during late pregnancy or nursing, causing transmammary infection of suckling pups and egg contamination of the environment once patency is established in the bitch. The bitch can reinfect herself by eating larvae from puppies' feces.


Clinical signs
In mild to severe infections, the pulmonary phase of larval migration is asymptomatic. Adults in the intestine induce tucked-up abdomen, stunted growth, vomiting, and diarrhea. Individual worms are sometimes vomited or excreted. Coughing, increased respiratory rate, and frothy nasal discharge are symptoms of heavy infections during larval migration.
Most T. canis deaths occur in the pulmonary phase, and puppies infected transplacentally may die within days after birth.
Diagnosis
While a larva is migrating, only a speculative diagnosis is achievable based on pneumonic symptoms in a litter—often within two weeks. In direct feces smears with a drop of water, the worms' egg production is so high that flotation is often unnecessary.
Treatment
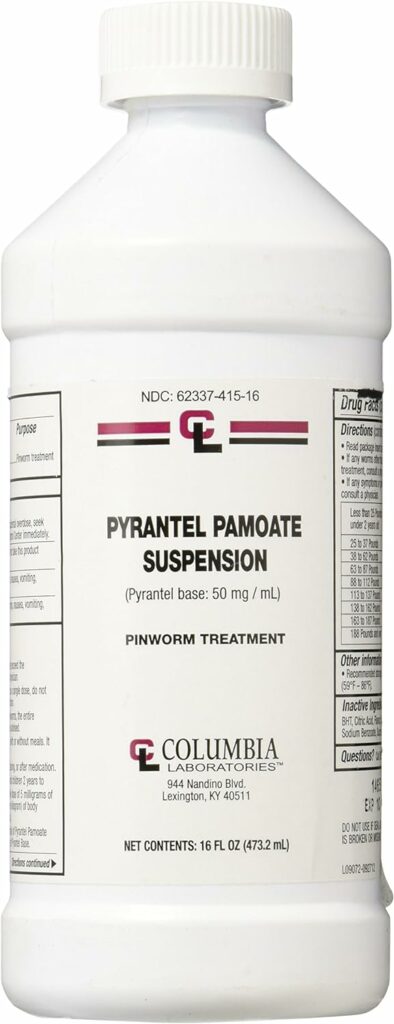
All puppies should be dosed with Prantel Pamoate (aka Strongid, Nemex) at two weeks and again every 2 weeks until 12 weeks old. Then, one per month until 6 months old. The dam should be treated at the same time as the puppies. Infection via the dam's milk or an increase in fecal egg production in the weeks following whelping should be treated with a second dose at two months.
It is suggested that adult dogs be treated every 3–6 months for worms.
Prevention
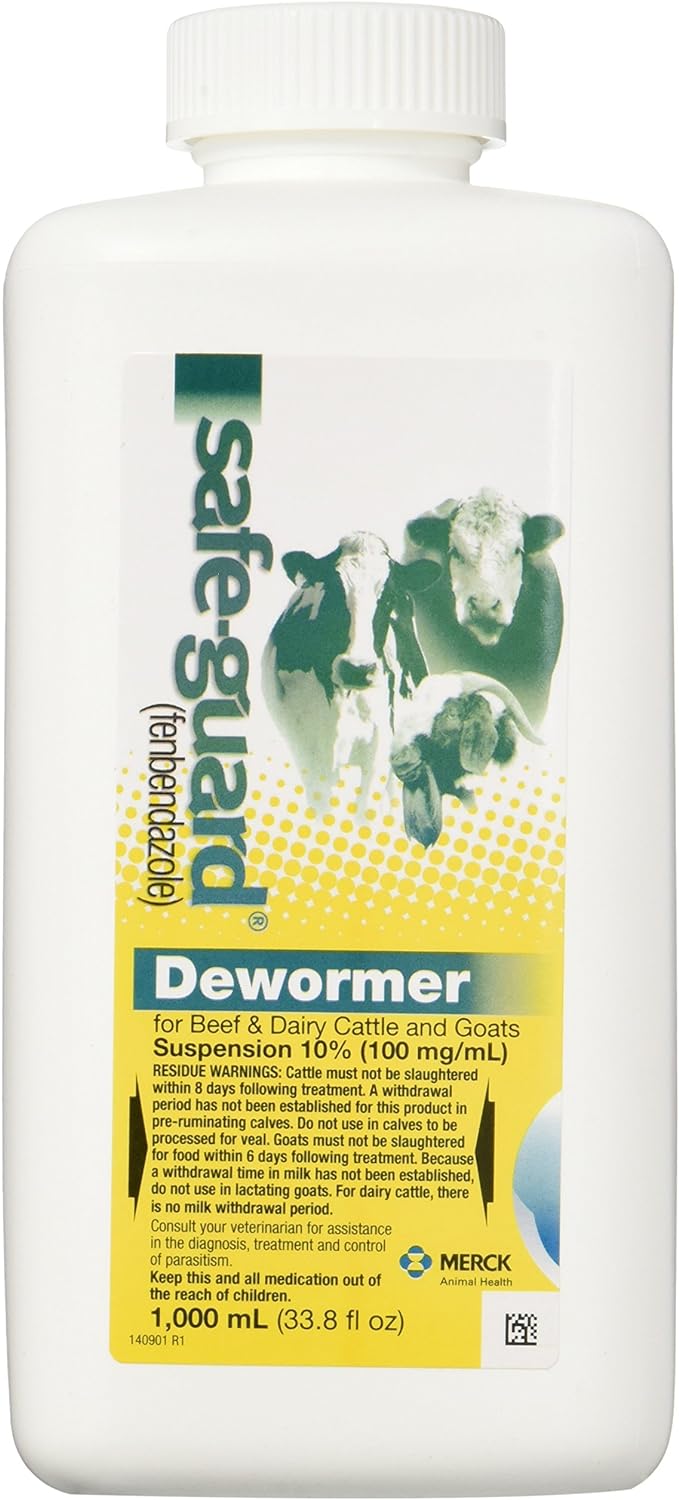
Fenbendazole for the last three weeks of her pregnancy through day 14 of lactation daily, that is five straight weeks. Give mom 50 mg/kg (pre-pregnancy weight) of Fenbendazole once every 24 hours. Also, CLEAN ALL FECES AS SOON AS POSSIBLE.
Fenbendazole (Panacur) kills MOST worms, but not all:
For dogs: 50 mg/kg (22.7 mg/lb) daily for three consecutive days for the removal of roundworms (Toxocara canis, Toxascaris leonina), hookworms (Ancylostoma caninum, Uncinaria stenocephala), whipworms (Trichuris vulpis) and tapeworms (Taenia piriformis). Also used to treat giardia (5-10 days for Giardia (Giardiasis) depending on severity.) DOES NOT KILL Flea tapeworm.
Repeat (3 daily doses ) in 2-3 weeks to kill off eggs that were not hatched during initial treatment.
Do NOT use on puppies under 6 weeks of age, but OK to use on the mother while pregnant and while nursing.
Hookworm (Ancylostoma caninum)
Ancylostoma caninum or canine hookworm is reddish-grey in appearance and is easily identified by the size and hook-like conformation. This parasite uses dogs, foxes and humans (cutaneous larva migrans) as hosts.

Clinical signs
Acute infections cause anemia, lassitude, and occasionally respiratory distress in sensitive animals exposed to high numbers of infective larvae. In suckled puppies, anemia is often severe, with diarrhea containing blood and mucus. Respiratory symptoms can be caused by larval lung injury or anemia's anoxic consequences. Chronic infections cause underweight, poor coat, loss of appetite, and, sometimes, pica.
Diagnosis
Hematological and fecal tests should support clinical signs and history. High feces worm egg counts can establish a diagnosis; however, suckling puppies may develop severe clinical indications before eggs are found in feces. A few hookworm eggs in the feces does not necessarily mean that a dog has hookworm disease.
Treatment
Same as for roundworms
Control
CLEAN ALL FECES quickly and give preventative worming.
Whipworm (Trichuris vulpis)
Tricuris vulpis, also known as whipworms, are whitish in color and have lengths of around 4.5–7.5 cm. This parasite stays in the large intestine of dogs and cats.

Clinical signs
Sporadic disease associated with severe infection is more common in dogs and causes acute or chronic cecal mucosal inflammation with bloody watery diarrhea. Anemia and weight loss are also possible.
Diagnosis
Since the clinical indications are not pathognomonic, detecting lemon-shaped Trichuris eggs in the feces may be diagnostic. Since clinical signs can arise during the prepatent phase, necropsy or a positive response to anthelmintic treatment may also be diagnostic. In addition, adult worms discharged in feces are rare.
Treatment
Panacur
Tapeworm (Dipylidium caninum) - NOT KILLED WITH PANACUR
Tapeworms have flat and segmented bodies. They may also be called double-pored or cucumber seed tapeworm due their appearance. Tapeworms adhere through the mouth to the host's intestinal wall. Worm segments break off and defecate out, typically sticking to the hair around the host's tail. They resemble moving rice grains and create anal inflammation.
Fleas and biting lice serve as intermediate hosts for this zoonotic tapeworm, which causes hydatidosis in infected humans.


Rodent Tapeworm (killed with panacur)

Clinical signs
An animal infested with worms may or may not display symptoms. Only if the infestation exceeds the host animal's resistance will the following symptoms appear:
- Anal irritation, scooting
- Itching
- Constantly hungry, eating but losing weight
- Vomiting and diarrhea
- Unhealthy, dull coat
- Enlarged abdomen (seen mainly in young animals)
Diagnosis
A section on the coat surrounding the perineum is often the first sign of infection. If a segment is new, the elongated shape and multiple genital organs can be seen with a hand lens that can help identify it. Dry and distorted segments must be broken up with mounted needles in water, allowing the egg packets to be observed under a microscope, distinguishing the segment from Taenia spp., which contains only several single oncospheres.
Treatment and Control
As with any infection, treatment and management must be implemented simultaneously. Insecticides should be used in conjunction with anthelmintics like nitroscanate and praziquantel. Insecticides should also be used on the animal's bedding and usual resting spots to eliminate the flea larvae that outnumber the adult parasites feeding on the animal.
Prevention
- Deworm regularly
- Control the intermediate hosts
- Dispose of feces immediately
- Disinfect where feces have been
- Wash hands thoroughly
- Wash animal bowls separately
- Do not let animals lick face
- Keep animal's anal area clean
- Examine feces regularly
Unit 2: Protozoa
These single-celled creatures, often found in water, have cell membranes and organelles (flagella and cilia) for movement. Binary fission is their method of reproduction, and their nutrition is holozoic. They can pursue prey by following a chemical trail or being stimulated by movement. On occasion, protozoa produce cysts—the phase that allows temporary survival outside the host.
Giardia
Giardia is a group of intestinal flagellated protozoan parasites infecting mammals, amphibians, and birds. A broad spectrum of hosts is infected by G. duodenalis, the most prevalent Giardia species, which causes chronic diarrhea.
Parasites in the intestines cause diarrhea through hypersecretion and malabsorption, affecting intestinal permeability. Most dogs and cats with Giardiasis show mild symptoms; however, some may experience diarrhea and weight loss, leading to chronic cases.

Clinical signs
Most Giardia shedders are subclinically infected. If the condition is chronic, the main symptoms are diarrhea, weight loss, and lethargy. Diarrhea is mucoid, soft to watery, and rarely bloody. It may be intermittent or continuous and can turn bloody in animals infected with Ancylostoma spp., Coccidia, or Tritrichomonas fetus.
Diagnosis
Giardia infection can be diagnosed by detecting cysts and trophozoites in fresh stool smears through direct examination or flotation cysts. Cysts can be concentrated using Sheather's sugar, formalin-ethyl acetate, or zinc sulfate centrifugation. As cysts are intermittently discharged, three consecutive samples are recommended. Moreover, immunochromatographic kits, immunofluorescence, Enzyme-Linked immunoassay (ELISA), and Polymerase Chain Reaction (PCR) can be used to detect the Giardia antigen rapidly.
Treatment
There are several effective treatments such as albendazole, fenbendazole, and metronidazole (aka Flagyl).

Control
Proper hygiene is required to prevent fecal contamination of feed and water since transmission is via feco-oral route.
Coccidia (Cystisospora canis)
Coccidia is an obligate intracellular parasite that belongs to the phylum Apicomplexa found in dogs' and cats' gastrointestinal tracts. Dogs serve as a definitive host for Cystoisospora canis, C. ohioensis, C. burrowsi, and C. neorivolta. The three latter species are collectively known as the C. ohioensis complex.
Clinical Signs
Puppies and kittens from dirty or overcrowded surroundings show more significant clinical signs. Cystoisospora spp. may produce large or small bowel diarrhea. Anemia, dehydration, vomiting, anorexia, and weight loss are often observed. Symptoms of Cystoisospora spp. infection includes abdominal pain, increased gas or fluid in the gastrointestinal tract, and thicker bowel loops.
Diagnosis
Postmortem coccidial stages in the intestines may identify coccidiosis. Animals experiencing diarrhea or dysentery may excrete oocysts. Oocysts are not diagnostic but should be investigated in conjunction with other indications of acute enteritis.
A coccidiosis diagnosis requires history, clinical symptoms, and organism detection. Centrifugal, fecal flotation or passive can identify oocysts.
Treatment
- Sulfadimethoxine
- Sulfadiazine/trimethoprim
- Amprolium
- Toltrazuril
Control
Sanitation and isolation can prevent coccidiosis. Daily cleaning is required in kennels and rescue centers. Standard disinfectants fail to kill coccidial oocysts, whereas ammonia-based treatments do.
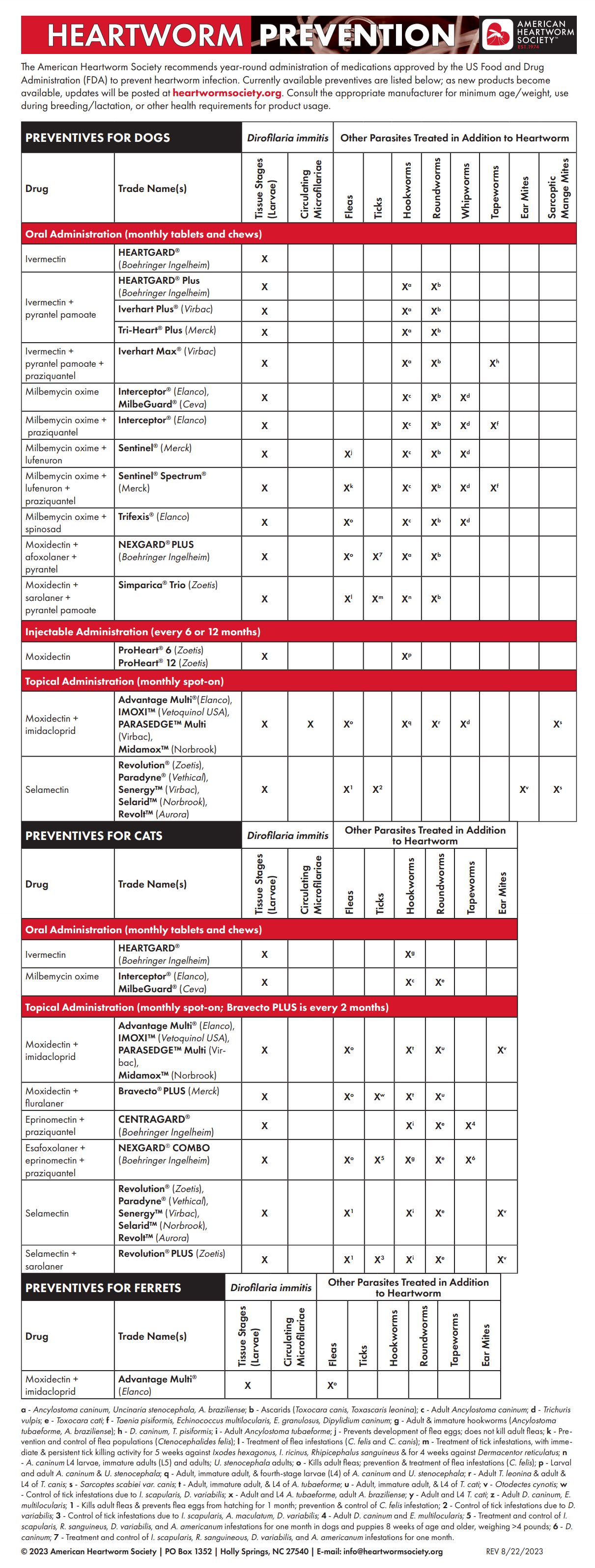
Unit 3: Heartworm (Dirofilaria immitis)
Adult canine heartworms can be found in the heart (right ventricle, right atrium) and adjacent blood vessels (pulmonary artery, posterior vena cava). This parasite uses mosquitoes as intermediate hosts.

Clinical signs
Dogs infected with canine heartworm show signs of restlessness and exercise intolerance. It can lead to chronic cough with hemoptysis and become dyspnea with edema and ascites in later stages of the disease.
Diagnosis
Initially, infected dogs are diagnosed based on clinical signs of cardiovascular dysfunction and presence of microfilaria in the blood. Dogs under one year of age are rarely diagnosed with this parasite given their long life cycle. In some cases, radiographic image of the thorax might show pulmonary artery thickness.
Immunodiagnostic techniques can also detect instances without detectable microfilaraemia. Most mature infections can be detected using antibodies, such as those found in some ELISA test kits for circulating heartworm antigens.
Treatment
An examination of the dog's heart, lung, liver, and kidney function is required before starting treatment. If these functions are grossly aberrant, heart insufficiency may need to be treated first. Infected dogs are usually treated intravenously with thiacetarsamide twice daily for two days or intramuscularly with melarsamide for two days to remove adult worms; toxic reactions are common due to dying disintegrating heartworms and embolism; activity should be restricted for 2–6 weeks. This treatment plan should be used with caution.
Six weeks later, different medicines should be used to treat microfilariae resistant to thiacetarsamide or melarsamide. The usual treatment is dithiazanine iodide or levamisole, taken orally over 10–14 days.
These drugs could harm microfilariae. Heartworms have been surgically removed in severe cases rather than risk drug-induced side effects. Following treatment, dogs are usually put on a preventive program.
Control
Because mosquito control is difficult, prophylaxis relies heavily on medication. In endemic locations, diethylcarbamazine is given orally to puppies daily at 2–3 months old.
In tropical places, the medicine is given all year, but in temperate zones, where the mosquito has a limited season, it is given one month before and two months after the mosquito season. It is important to check for microfilaria before starting prophylaxis in older dogs or after treating an infected dog since anaphylaxis can happen in infected dogs treated with diethylcarbamazine. Once prophylaxis is started, check for microfilariae every six months.
It is relatively safe to double the dose.
- up to 14 pounds: 1 drop (0.05 cc)
- 15 to 29 pounds: 0.1 cc
- 30 to 58 pounds: 0.2 cc
- 59 to 88 pounds: 0.3 cc
- 89 to 117 pounds: 0.4 cc
- 118 to 147 pounds: 0.5 cc
Beware of MDR1 mutation - Collie Breeds



Responses